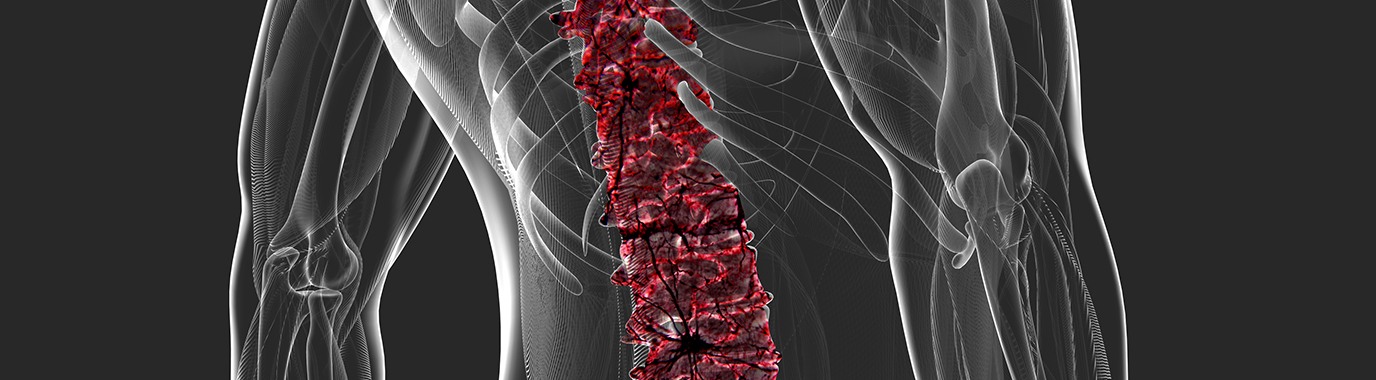
Chronic low back pain (CLBP)
Chronic low back pain is defined as the pain that persists for 12 weeks or longer after an injury, disease or stress on different structures of the body. Pain persists with varied intensity from mild to severe.
90% of CLBP cases cannot be attributed to a pathoanatomic cause and are thus referred to as ‘non-specific’.2 53% of patients have to wait more than one year to get the right diagnosis of the cause of their pain.3 64% of patients have to wait more than one year to get adequate pain management.3
It is our ambition to increase responder rates in a stratified sub-population and slow or reverse progression of chronic pain.
We therefore see a need for:
- Increasing responder rates in stratified sub-populations with targeted treatments that consider the pathological process of CLBP to shorten the time to diagnosis and appropriate pain management.
- Improving functional endpoints in a stratified sub-population where e.g. avoidance of interventional procedures would create significant benefits to the patient
Disease Overview
Definition and symptoms
CLBP patients not only experience personal distress and pain, but also present with significant sleep disorders and disability.2 CLBP symptoms include stiffness and muscle tenderness.4 Non-specific terms, such as strain, sprain or degenerative processes, are commonly used. Strain and sprain have never been anatomically or histologically characterised, and patients given these diagnoses might accurately be said to have idiopathic LBP.5,6
Epidemiology and risk factors
CLBP is in the top 5 most prevalent disorders in the EU, with an estimated prevalence of 25M.7 In the US, prevalence has risen in the last decade from 3.9% to 10.2% (32M) of the population.8 Some of the main risk factors for CLBP are occupational hazards e.g. jobs that require repetitive bending, sedentary lifestyle, excess weight and poor posture.9
Current management approaches
Pharmacological approaches for CLBP include antidepressants10 and a variety of opioids.11
References
- Andersson GBJ. The Adult Spine: Principles and Practice. Philadelphia: Lippincott-Raven; 1997:93–141.
- Deyo RA, Weinstein JN. N Eng J Med 2001;344(5):363–70.
- InSites Consulting. Pain Proposal Patient Survey. July – September 2010 https://www.dgss.org/fileadmin/pdf/Pain_Proposal_European_Consensus_Report.pdf
- Hayashi Y. JMAJ 2004;47(5):227–33.
- Hart LG, et al. Spine 1995;20(1):11–9.
- Deyo RA, et al. JAMA (Chic III) 1992;268(6):760–5.
- Juniper M et al. Expert Opin Pharmacother 2009;10(16):2581–92.
- Freburger JK, et al. Arch Intern Med 2009;169(3):251–8.
- Manchikanti L et al. Pain Physician 2009;12:E35–70.
- Schnitzer TJ, et al. J Pain Symptom Manag 2004;28(1):72–95.
- Chou R, Huffman LH. American Pain Society: Clinical Guideline for Evaluation and Management of Low Back Pain. Evidence Review. Glenview, IL, 2007.
- Ballantyne JC. JAMA Intern Med. 2016;321(22):2459–60.
Our therapeutic areas
Chronic post-surgical pain
Osteoarthritis

If you are interested in collaborating with us...
Contact us