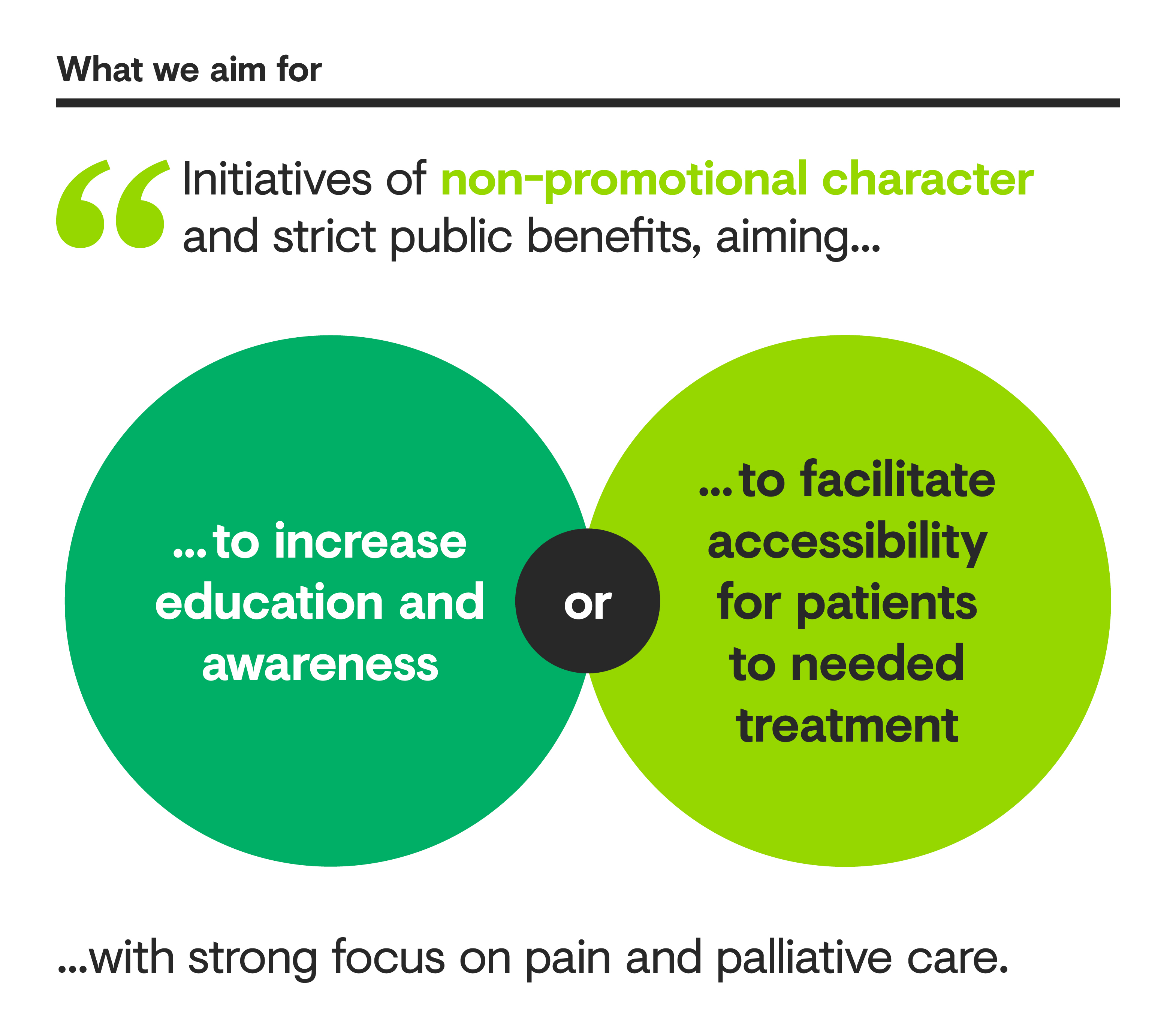
Impact Initiative: Education on Responsible Use of Pain Medication
We have a longstanding tradition of educating healthcare professionals about pain management to deepen understanding of patients’ needs, as well as the risks and benefits of pain medication. This Impact Initiative places an even stronger focus on this topic.