Peripheral neuropathic pain
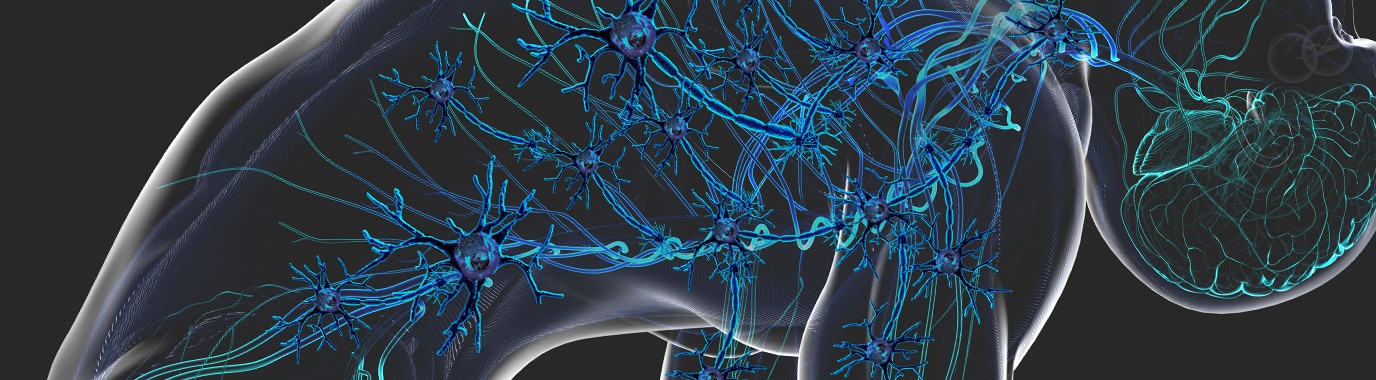
Peripheral neuropathy involves damage to the nervous system that receives stimuli from all parts of the body and transmits them via the spine to the brain where they are interpreted - for example as painful sensations.
The condition can occur as a result of chemotherapy and radiotherapy, or as a post-surgical complication, but the most frequent cause is nerve damage associated with diabetes (Diabetic Polyneuropathy). It is estimated that around 5 million people in the US and the five largest EU countries have a formal diagnosis for a peripheral neuropathy, and around half of these patients experience pain or discomfort, e.g. paraesthesia. However, current treatments are often unable to provide relief quickly – if at all.
We therefore see a need for:
- Superior responder rates with non-inferior effect size to standard of care that is achieved with fewer dose adjustments
- Ability to stratify patient population into responders and non-responders
- Rapid acting pain control for onset of sharp, unpredictable flares for neuropathic pain
Disease overview
Definition and symptoms
An essential element of neuropathic pain is the combination of sensory loss with hypersensitivity in the painful area.1 The nerves in the extremities (hands, arms, feet and legs) are damaged and the symptoms depend on which nerves are affected. PNP is characterised by abnormal and unpleasant positive e.g. shooting, stabbing or numbness and negative e.g. loss of thermal perception symptoms.2,3
Epidemiology and risk factors
PNP is a highly prevalent condition, accounting for 40% of all neuropathic pain cases.3 The peripheral neuropathy underlying the neuropathic pain can have several causes, most prominently hyperglycaemia due to diabetes (diabetic peripheral neuropathy: DPN)4 or cancer treatment via chemotherapy (chemotherapy induced neuropathy: CIPN) or radiotherapy (radiotherapy induced peripheral neuropathy: RIPN).5
Current management approaches
Owing to the heterogeneity of PNP, current PNP treatments are limited by systemic side effects and a lack of analgesic response to treatments.6,7 Depending on the cause of peripheral neuropathy, the management approach varies.
References
- Jensen TS, et al. Curr Opin Neurol. 2009;22:467‒74.
- IASP Taxonomy Working Group. Classification of Chronic Pain, Second Edition (Revised). Part III Pain Terms. IASP Press; 2011.
- Mick G, et al. Pain Manag. 2012;2:71‒7.
- Callaghan BC, et al. Lancet Neurol. 2012;11:521–34.
- Bennett MI, et al. Pain. 2019;160:38–44.
- Stillman M. Cleve Clin J Med. 2006;73(8):726–39.
- Colloca L, et al. Nat Rev Dis Primers. 2017;3:17002.
- Schreiber AK, et al. World J Diabetes 2015;6(3):432-44.
- Hershman DL, et al. J Clin Oncol 2014;2(18):1941–67.
Our therapeutic areas
Chronic low back pain
Osteoarthritis

If you are interested in collaborating with us...
Contact us