
Pain Management
Managing pain responsibly
Are NSAIDs compatible with other pain medications/analgesics?
Synergistic interactions of drugs that target different pain mechanisms might provide enhanced analgesia with fewer side effects compared with higher monotherapy doses. However, evidence supporting a combination pharmacotherapy approach in chronic pain management is limited.1
Co-administration of NSAIDs with commonly used medications, including some other pain medications, can result in drug–drug interactions and adverse drug reactions. When assessing the risk of a patient taking an NSAID, the type of concomitant medication being taken, if any, is an important factor to consider.2–4
Please see What are the main risks cautions and contraindications when using NSAIDs? for more information.
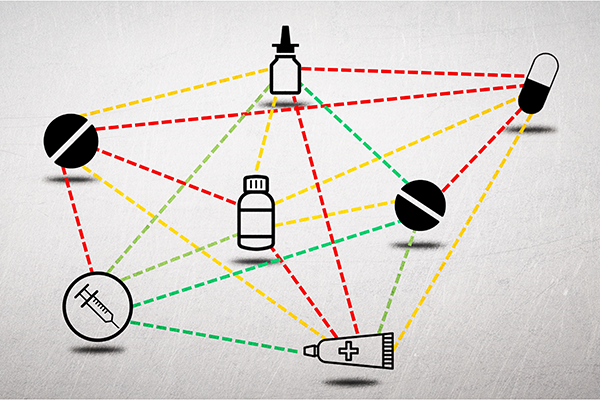
Illustrating which pain medications NSAIDs can be used with using a traffic light system
In this section, we have developed a traffic light system in which:
- Green means the medication has not been shown to increase risk of NSAID-related side effects and can benefit some patients. These medications still incur risks of their own
- Orange means the medication incurs an increased risk of NSAID-related side effects
- Red means that there is a contraindication to the co-administration of the two analgesic medications
Although not appropriate for every situation, the World Health Organization analgesic ladder for the management of cancer pain provides a good framework for considering pain medication combinations. Step 1 starts with the use of non-opioid analgesics, such as paracetamol and systemic NSAIDs.Systemic NSAIDs are one of the more commonly sold over-the-counter (OTC) and prescribed classes of medication. The analgesic ladder builds up to the inclusion of opioids, if appropriate, with or without co-administration of adjuvants at each step4–7.Adjuvants include the following6,7:
- Tricyclic antidepressants and selective serotonin/norepinephrine reuptake inhibitors (SSRIs/SNRIs)
- Anticonvulsants
- Topical anaesthetics and therapies
- Corticosteroids
- Cannabinoids
NSAIDs and paracetamol are commonly used in combination and have a potentially synergistic analgesic effect8,9,and can also be taken at the same time as ketamine10,11.
NSAIDs are also often used in combination with opioids owing to their additive analgesic effects, and fixed-dose combinations of NSAIDs with opioids are available1,7.NSAID use has been associated with reduced opioid consumption and improved postoperative pain8.Please use this link for information about the responsible use of opioids.
Two or more systemic NSAIDs should not be used in combination,12 and patients should be counselled to avoid taking over-the-counter NSAID preparations when taking an NSAID.12 While topical NSAIDs are available, caution is needed when co-prescribing these products with a systemic NSAID13,14.
Use of low-dose aspirin in combination with a non-aspirin NSAID should also be carefully considered because this may increase the risk of gastrointestinal (GI) bleeding and antagonise the anti-platelet effect, potentially allowing clot formation2,15.
- For more information, see article titled "Should an NSAID be prescribed with a gastroprotective agent?"
The risk of bleeding may also be increased when NSAIDs are combined with tricyclic antidepressants, such as amitriptyline and venlafaxine,15 as well as when combined with an SSRI/SNRI (e.g. fluoxetine)15-17.Additionally, use with oral corticosteroids may also increase the risk for serious GI toxicity15,18.
Caution is required when combining cannabinoids with NSAIDs, as there is a potential for increased accumulation of the NSAID in the serum which may elevate the risk of an adverse event.19,20
Co-prescribing NSAIDs with anticonvulsants (e.g. gabapentin, pregabalin, valproate) should be done cautiously as this combination may lead to displacement of the anticonvulsant and/or NSAID from plasma binding-sites, leading to increased free concentrations that may increase the risk of a drug-associated adverse event21,22.
This article only covers NSAID interactions with pain medication, and healthcare professionals should also check for potential drug interactions with NSAIDs and non-pain medications, whether prescribed or over the counter23.
Further reading
For further information on pain medications, including NSAIDs, please refer to:
- Medline Plus. US National Library of Medicine. Pain relievers. Available at: https://www.nlm.nih.gov/medlineplus/painrelievers.html. Accessed August 2022.
- American Academy of Family Physicians. Pain relievers: understanding your OTC options. Available at: http://familydoctor.org/familydoctor/en/drugs-procedures-devices/over-the-counter/pain-relievers-understanding-your-otc-options.html. Accessed August 2022.

Dr Raúl Marques Pereira
General Practitioner, Portugal

Dr Beatriz Craveiro Lopes
Anaesthesiologist, Portugal
-
References
1. Gilron I, et al. Lancet Neurol. 2013;12:1084–95.
2. Moore N, et al. Ther Clin Risk Manag. 2015;11:1061−75.
3. National Institute for Health and Care Excellence. NSAIDs – prescribing issues. April 2020. Available at: https://cks.nice.org.uk/topics/nsaids-prescribing-issues/. Accessed August 2022.
4. Szeto CC, et al. Gut. 2020;69:617–29.
5. White WB, et al. J Cardiovasc Pharmacol Ther. 2018;23:103–18.
6. Anekar AA, Cascella M. WHO analgesic ladder. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; May 2022. Available at: https://pubmed.ncbi.nlm.nih.gov/32119322/. Accessed August 2022.
7. The World Health Organisation. Cancer Pain Relief. Geneva. 1986. Available from: https://apps.who.int/iris/bitstream/handle/10665/43944/9241561009_eng.pdf. Accessed August 2022.
8. Cheung CK, et al. J Pain Res. 2022;15:123–35.
9. Ong KS, et al. Anesth Analg. 2010;110:1170–9.
10. Cohen SP, et al. Reg Anesth Pain Med. 2018;43:521–46.
11. Ketamine for pain. Newcastle upon Tyne Hospitals NHS Foundation Trust. December 2015. Available at: https://www.palliativedrugs.com/download/140114_Ketamine_for_pain.2013.FINAL.PIL.pdf. Accessed August 2022.
12. Garcia Rodríguez LA & Hernández-Díaz S. Arthritis Res. 2001;3:98–101.
13. Dimassi AI, et al. Springerplus. 2016;5:1236.
14. PENNSAID (diclofenac sodium topical solution 2% w/w). Prescribing Information (US)
15. Masclee GM, et al. Gastroenterology. 2014;147:784–92.e9.
16. Perahia DG, et al. Drug Healthc Patient Saf. 2013 Nov 25;5:211–9.
17. Anglin R, et al. Am J Gastroenterol. 2014;109:811–19.
18. Piper JM, et al. Ann Intern Med. 1991;114:735–40.
19. Wilson-Morkeh H, et al. Rheumatology (Oxford). 2020;59:249–51.
20. Emig M, et al. J Neurol Res. 2020;10:132–5.
21. Sandson NB, et al. Am J Psychiatry. 2006;163:1891–6.
22. Hurley RW, et al. Anesthesiology.
23. Naproxen 500 mg tablets. Summary of Product Characteristics. Updated October 2021. Available at: https://www.medicines.org.uk/emc/product/5823/smpc. Accessed August 2022. Clinard F, et al. Eur J Clin Pharmacol. 2004;60:279–83.
Disclaimers
Please be aware:
- Prescribing information in various geographies may differ and therefore you may be exposed to information that is outside the licensed label for your region. For up-to-date information on medicinal agents in the country where you are practicing, please refer to country-specific product information.
- Prescription of any medication is at the sole discretion of the treating physician, who should consider all the characteristics and needs of the individual patient, with due regard for any local treatment guidelines.
- Note that articles shared here may include links to third-party websites, services or content. Your browsing and interactions on any other websites, or your dealings with any other third party service provider, is subject to that website’s or third party service provider’s own rules and policies. We encourage you to consult the privacy statements of the providers whose services and/or content we link to and who are responsible for the content provided and the protection of your data in this context. Grünenthal does not monitor, control or endorse the privacy practices of any third parties. Please refer to our privacy statement for more information.