Key Pain Conditions
Many chronic conditions are challenging to manage. Here we focus on key pain conditions with a high unmet need among patients and/or healthcare professionals.
Our aim here is to provide the pain community with in-depth information about these conditions; from disease understanding to management approaches.
Neuropathic back pain
Like many chronic pain conditions, chronic back pain can have nociceptive, neuropathic and nociplastic components.1–3 The neuropathic component of chronic back pain is under-recognised; it can arise from an injury or disease that directly affects the nerve roots of the spine and lower limbs, and the pathological invasive nerve supply of damaged discs in the lumbar region.4 Neuropathic back pain (NBP) is associated with an increased likelihood and severity of medical comorbidities as well as higher healthcare costs compared with back pain without a neuropathic component.4
[Throughout this article when we mention back pain, we are predominantly referring to pain in the lower back. You can read about chronic low back pain here
Quick facts
- Chronic back pain is considered to be a mixed pain syndrome, consisting of nociceptive, neuropathic and nociplastic components.1–3
- Estimates suggest that 5–55% of patients with chronic low back pain have a neuropathic pain component.4
- A number of pathophysiological mechanisms have been implicated in NBP, including lesions to nociceptive sprouts, mechanical compression and inflammation to the nerve roots.4
- Numerous comorbidities affecting the nervous system can lead to NBP, including tumours that compress the spinal cord, herpes zoster infection and neurodegenerative diseases such as multiple sclerosis.5,6
- NBP is a burden on patients and healthcare systems, causing pain, poor quality of life and reduced work productivity.7–9
- NBP symptoms include paroxysmal (e.g. shooting or stabbing) and dysaesthetic (unpleasant sensations such as prickling or crawling) pain, and/or pain associated with abnormal thermal sensations (e.g. burning).4,7
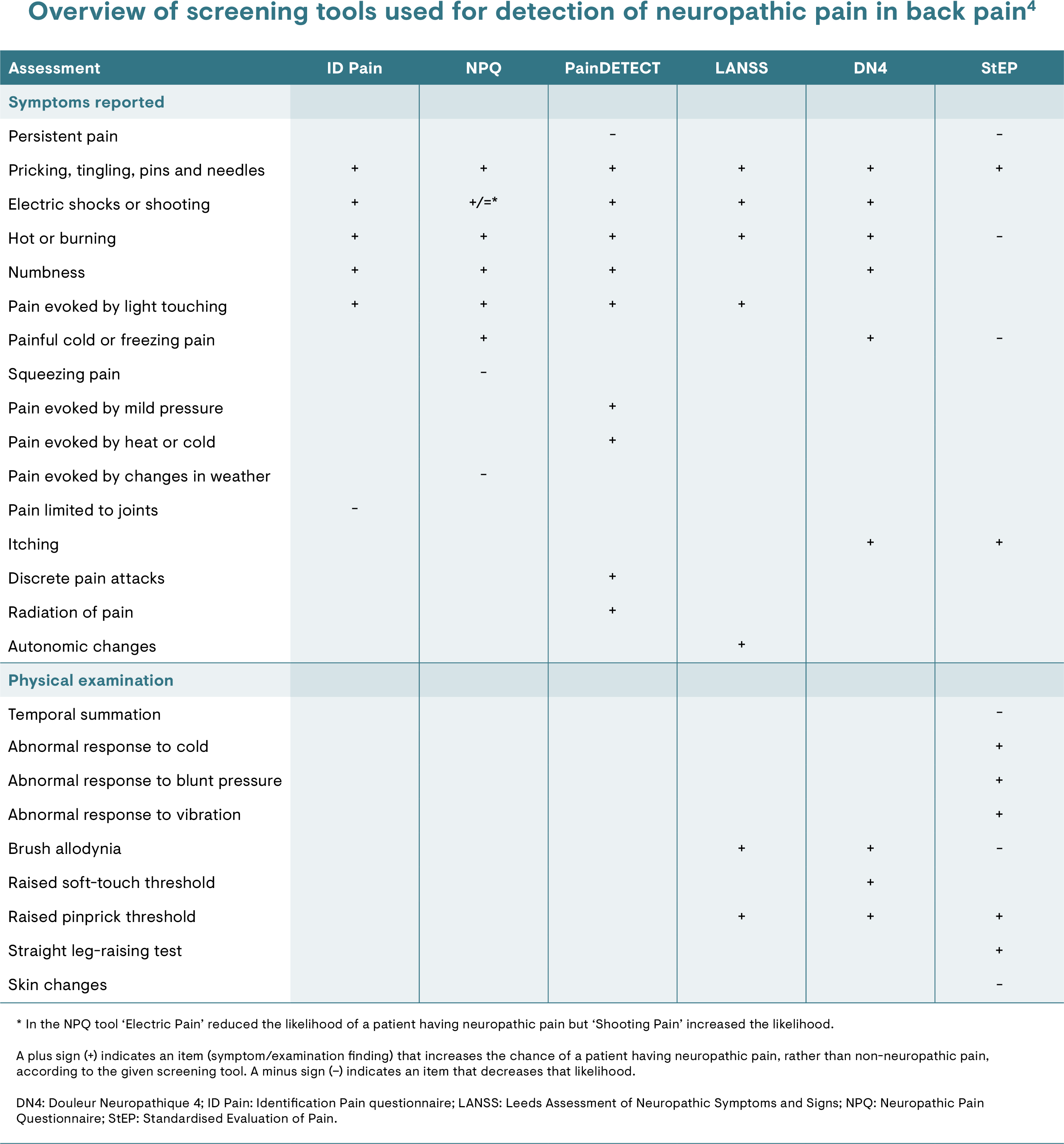
- Douleur Neuropathique en 4 Questions (DN4) questionnaire, PainDETECT questionnaire and the Standardised Evaluation of Pain (StEP) questionnaire are validated screening tools available to facilitate the identification of a neuropathic pain component of chronic back low pain.4
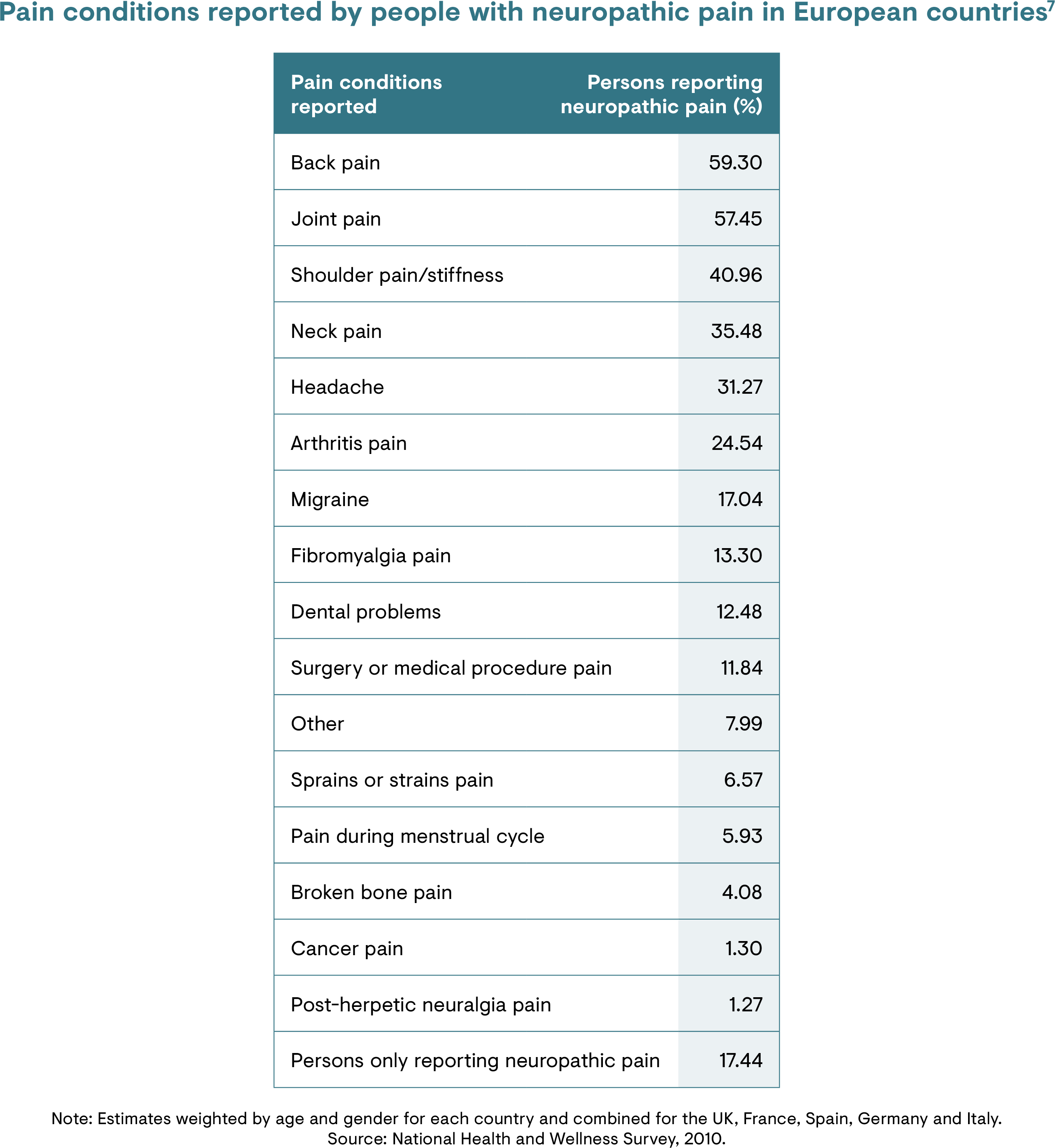
Epidemiology
Chronic back pain is often a mixed pain syndrome, arising from nociceptive and/or neuropathic pain.4,10 Studies indicate the presence of a neuropathic pain component in 5–55% of patients with chronic back pain.4 Pain in the back is the most common pain condition reported by patients with neuropathic pain, with chronic lumbar radicular pain affecting 20–35% of patients with back pain.7
NBP is associated with an increased likelihood and severity of medical comorbidities as well as higher healthcare costs compared with back pain without a neuropathic component.4 An analysis of a US claims database found that the mean annual per-patient cost of care was approximately 160% higher in patients with NBP than those without neuropathic pain.11
Risk factors
There are many potential risk factors that contribute to NBP as it can arise from different underlying diseases, conditions or injuries. It is known that neuropathic pain is more frequent in women and people >50 years of age.12 Psychological factors also play a role in the development of chronic back pain.13
[You can read more about the risk factors for chronic low back pain here
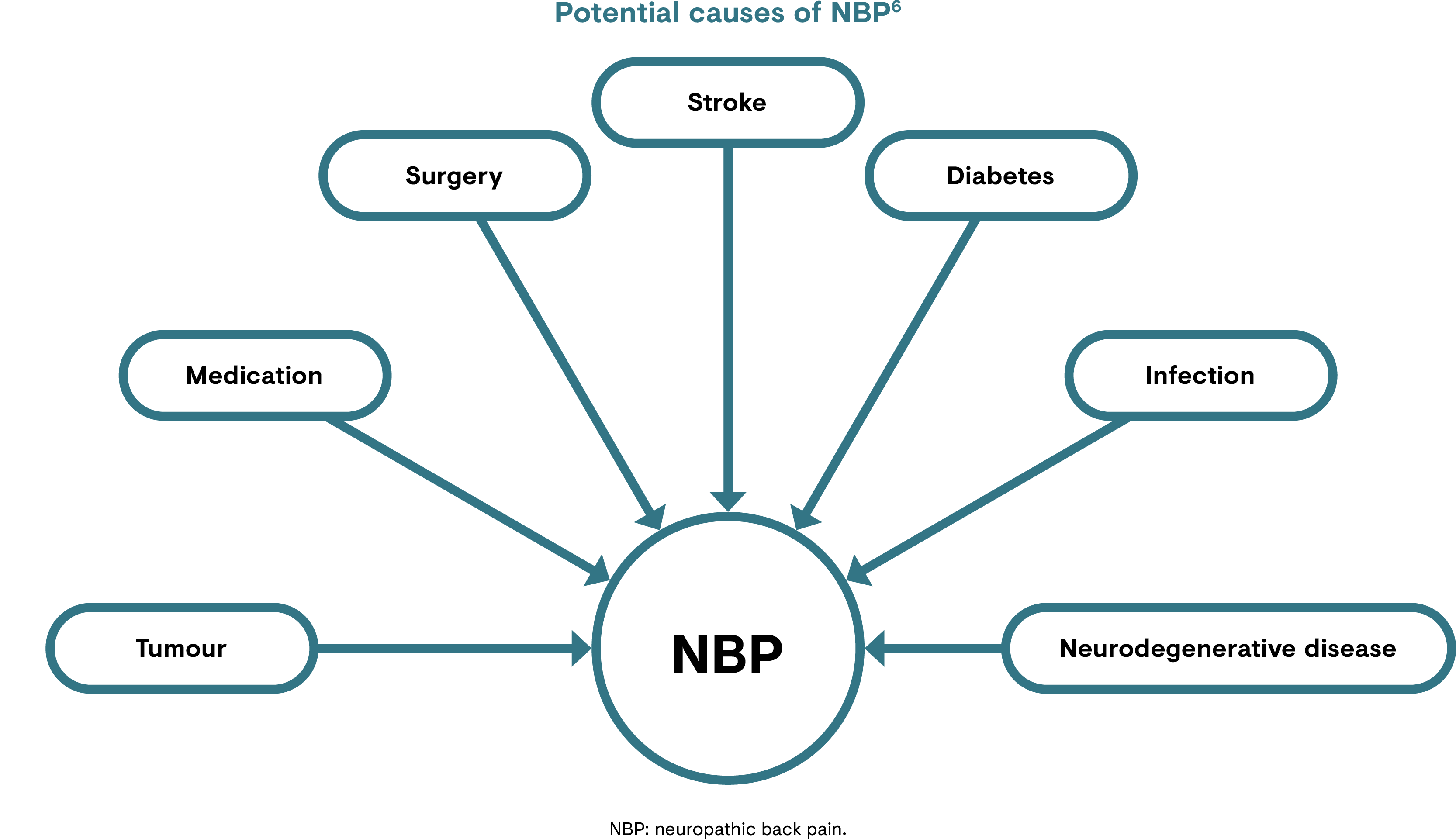
Causes
Neuropathic pain is defined as pain caused by a lesion or disease of the somatosensory nervous system.14,15 The cause of NBP can arise from a number of different sources.7 Chronic pain also occurs in neurological conditions of unknown aetiology, i.e. idiopathic neuropathies.6 Conditions or events contributing to the somatosensory lesion may include:4,6,7,16
- Tumours compressing a peripheral nerve or the spinal cord
- Physical injury such as a prolapsed or herniated disc and sprained muscular conditions
- Surgery that leads to failed back surgery syndrome
- Pain arising post-stroke
- Comorbidities such as diabetes
- Local or systemic inflammation
- Viral infection such as herpes zoster
- Neurodegenerative diseases such as multiple sclerosis
Signs and symptoms
Migraine is characterised by headache lasting between 4–72 hours of pulsating quality associated with nausea and/or photophobia and phonophobia.2
Characteristics of NBP vary between patients and over time,4 but a common denominator is that people with NBP typically experience higher levels of pain and lower quality of life compared with those with nociceptive back pain.7,8 A study of patients across Europe showed that around 50% of people reporting NBP were impaired in their work,9 while another study showed that 38% of people with neuropathic pain reported severe daily pain.8
Painful signs and symptoms in an area of altered sensation suggest neuropathic pain.4 Spontaneous pain in NBP may be paroxysmal (e.g. shooting or stabbing), dysaesthetic (unpleasant sensations such as prickling or crawling) and/or associated with abnormal thermal sensations (e.g. burning).4,7
Pathophysiology
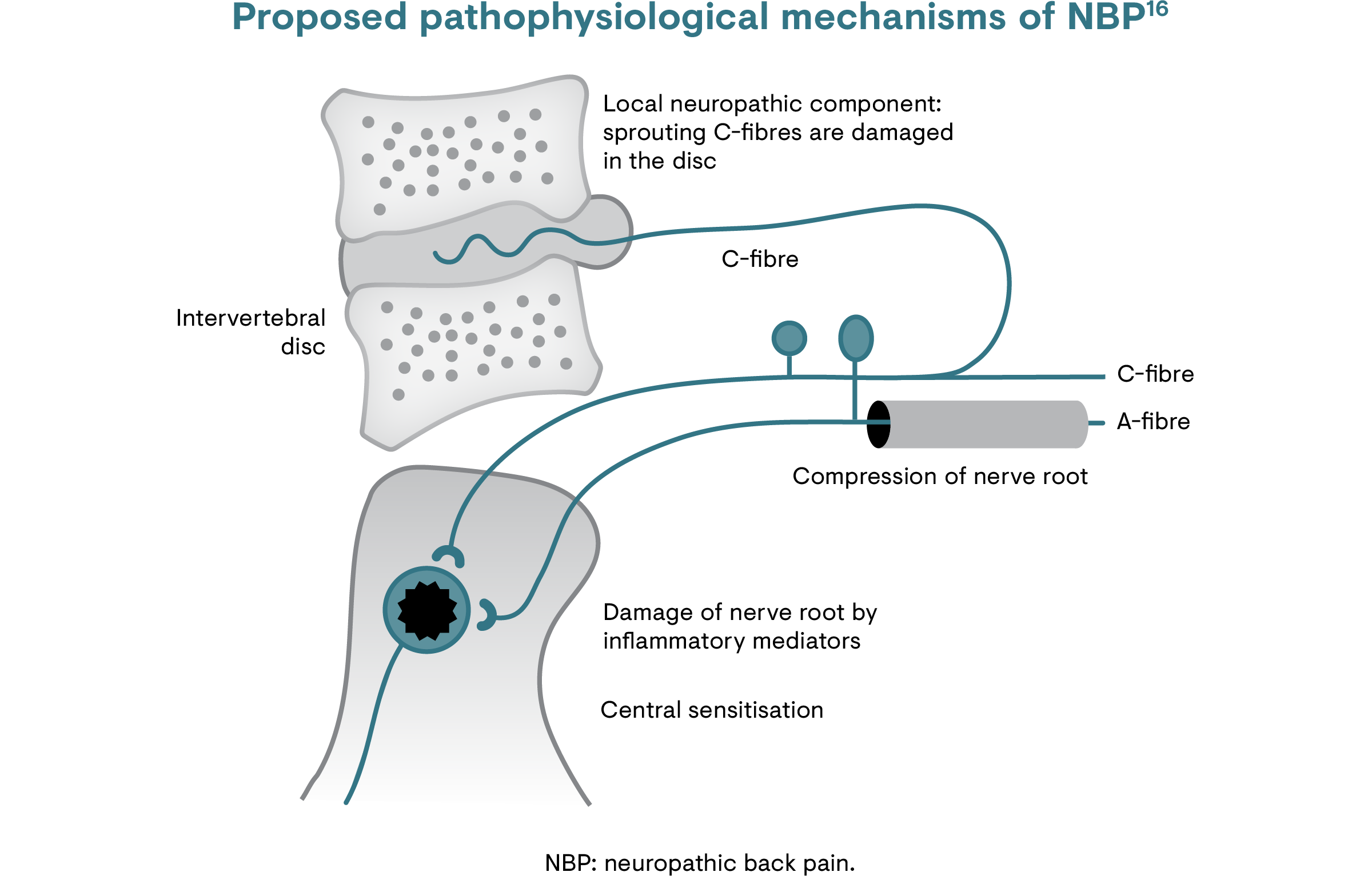
The precise mechanisms of neuropathic pain are not completely understood. In chronic back pain, neuropathic pain may be caused by several mechanisms in the spinal axis:4,16
- Lesions of nociceptive sprouts within a degenerated disc
- Mechanical compression of the nerve root
- Effects of inflammatory mediators arising from a degenerative disc that result in inflammation and damage to the nerve roots
Pain may arise from mechanical stress, which stimulates production of inflammatory agents such as cytokines and chemokines.16 Inflammatory mediators may reach nerve fibres that are not mechanically affected.16 In addition, sensitisation of the peripheral nerves or roots may lead to secondary sensitisation of spinal cord neurons, amplifying abnormal pain processes.16
Diagnosis
According to the International Classification of Diseases 11th Revision (ICD-11), the diagnosis of chronic NBP requires a history of nervous system injury or disease and a neuroanatomically plausible distribution of the pain.6 Sensory signs and symptoms such as decreased or loss of sensation, allodynia or hyperalgesia, indicating the involvement of the somatosensory nervous system, must be compatible with the area of the affected nervous structure.6
Clinical examination of a patient with suspected NBP should investigate possible sites of an underlying somatosensory lesion.7 This will inform further diagnostic investigations, such as electrodiagnostic techniques, myelography, computed tomography and magnetic resonance imaging, to identify causative pathologies within the nervous system.7
Tools such as the PainDETECT questionnaire have been used to demonstrate clinical characteristics that differentiate the neuropathic component of chronic back pain from other types of pain (i.e. nociceptive).17
[Learn more about screening tools for neuropathic pain in the article on peripheral neuropathic pain
Management
Guidelines and recommendations
Guidelines for chronic back pain and neuropathic pain typically do not include recommendations specifically for NBP, and there is no standardised algorithm for identifying NBP.4 The UK’s National Institute for Health and Care Excellence (NICE) and the Belgian Health Care Knowledge Centre have developed guidelines for the management of sciatica and radicular pain, respectively:18,19
- Low back pain and sciatica in over 16s: Assessment and management
- Low back pain and radicular pain: Assessment and management
Treatment must be personalised based the characteristics of each patient’s condition, including their symptoms, comorbidities, risk profile and cost.4 Multimodal management of chronic back pain, combining pharmacological therapies for symptomatic relief with non-pharmacological approaches, such as physical activity and psychosocial/behavioural interventions, is generally recommended.4
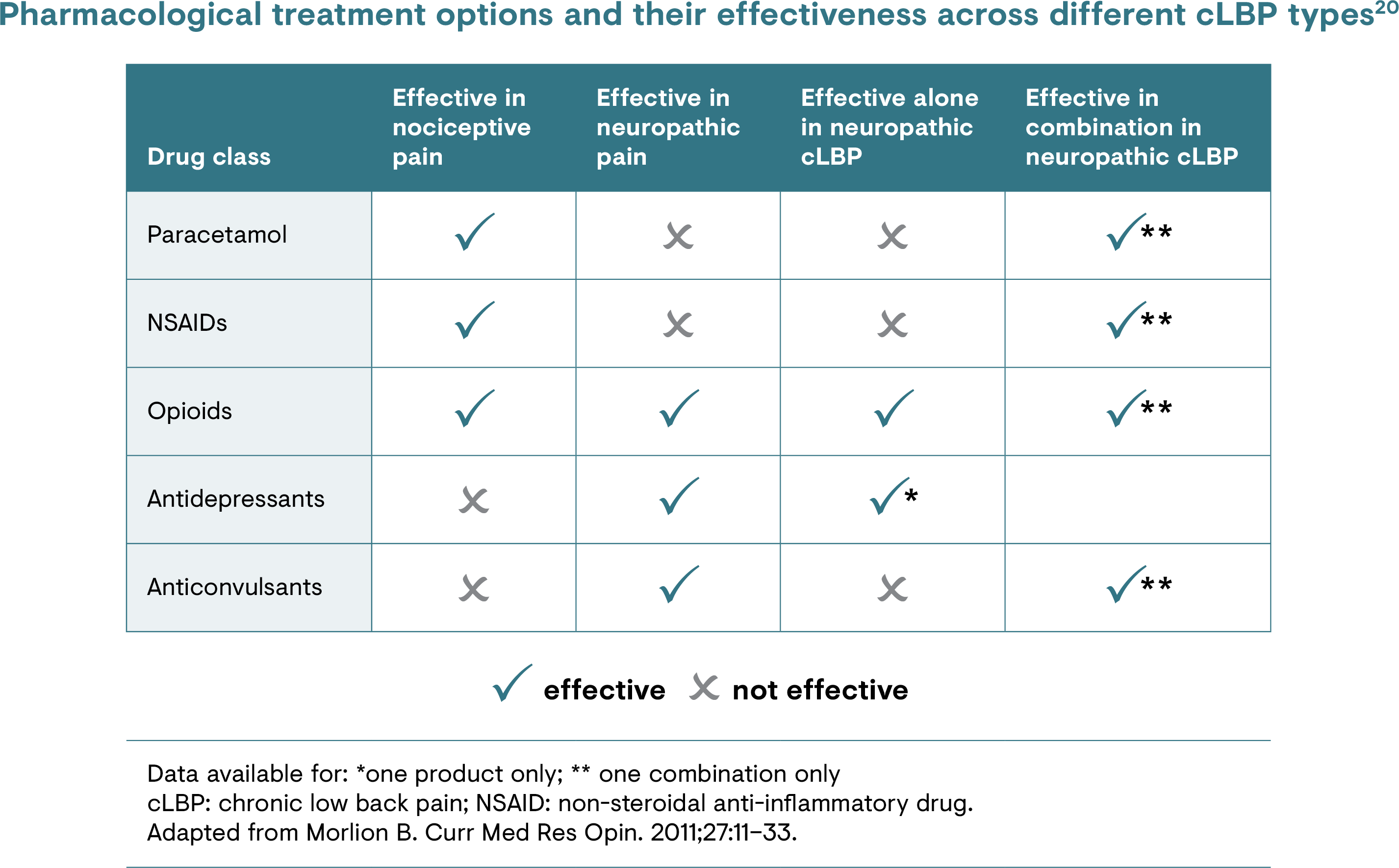
Pharmacological treatments
Guidance on the use of paracetamol for managing back pain, either alone or in combination with other agents, varies between guidelines.4,5,10,18,19 Non-steroidal anti-inflammatory drugs are also commonly used for back pain but these provide little relief of a neuropathic pain component.4,5 Benzodiazepines, systemic corticosteroids, antidepressant medications, anti-epileptic drugs, skeletal muscle relaxants and opioid analgesics are also prescribed.4,10 Monotherapy with most of these agents typically provides only limited relief of neuropathic pain.10 Evidence suggests that some opioid and topical analgesics may be effective in NBP in defined patient populations, but more well-designed trials are needed.4
[Please refer to the section on chronic low back pain
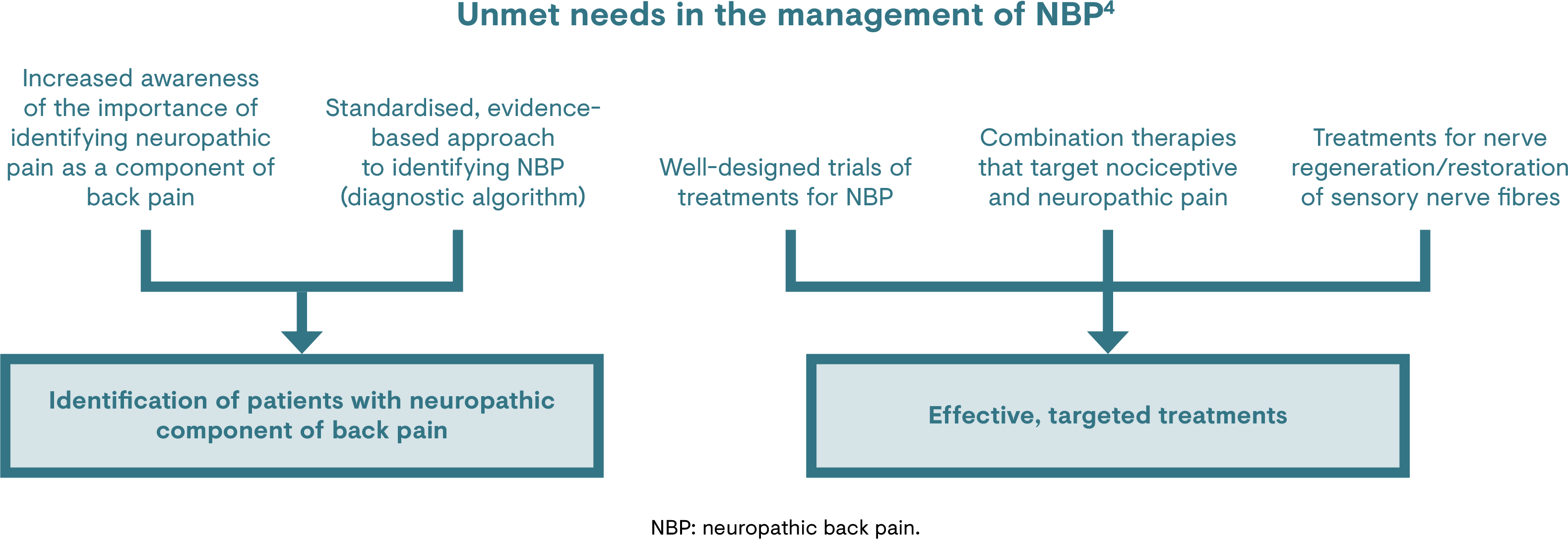
Unmet needs
The neuropathic component of back pain is under-recognised, under-treated and difficult to manage.4 Experts point out a lack of standardised recommendations for diagnosis of the neuropathic component of back pain, and of specific guidelines on its management.4
There is a need for improved treatment options for the management of the neuropathic component of chronic back pain, particularly as patients with a neuropathic component have disproportionately higher healthcare costs (vs those without neuropathic pain).4,11 Unfortunately, few clinical trials have investigated important aspects of back pain management including nerve regeneration/restoration of sensory nerve fibres (i.e. disease modification), the suitability of combinations that target nociceptive and neuropathic pain, or head-to-head comparisons of treatments.4,10,21 Well-designed trials could help to inform algorithms for the diagnosis and treatment of NBP, and to explore the use of combination therapies to improve patient outcomes.5
-
References
1. Morlion B. Nat Rev Neurol. 2013;9(8):462–73.
2. Kosek E et al. Pain. 2016;157(7):1382–86.
3. Trouvin AP & Perrot S. Best Pract Res Clin Rheumatol. 2019;33(3).
4. Baron R et al. Eur J Pain. 2016;20(6):861–73.
5. Mick G et al. Curr Med Res Opin. 2020;37(2).
6. Scholz J et al. Pain 2019;160:53–9.
7. Nijs J et al. Pain Physician. 2015;18(3):E333–E346.
8. Langley PC et al. J Med Econ. 2013;16(1):85–95.
9. Liedgens H et al. Clin Outcomes Res. 2016;8:113–26.
10. Romanò CL et al. Pain Res Treat. 2012;2021:154781.
11. Mehra M et al. J Med Econ. 2012;15(2):245–52.
12. Bouhassira D et al. Pain. 2008;136(3):380–7.
13. Ehrlich GE. Bull World Health Organ. 2003;81:671–6.
14. Jensen TS et al. Pain. 2011;152(10):2204-5.
15. Treede RD et al. Neurology. 2008;70(18):1630–5.
16. Freynhagen R & Baron R. Curr Pain Headache Rep. 2009;13(3):185–90.
17. Spahr N et al. Musculoskelet Sci Pract. 2017;27:40-48.
18. National Institute for Health and Care Excellence (NICE). Low back pain and sciatica in over 16s: Assessment and management NICE guideline. 2020. Available at: www.nice.org.uk/guidance/ng59. Accessed June 2021.
19. Van Wambeke P et al. Low Back Pain and Radicular Pain: Assessment and Management. 2017. Available from: www.kce.fgov.be. Accessed June 2021.
20. Müller-Schwefe G et al. Curr Med Res Opin 2011;27:481–8.
21. Anand P et al. J Pain Res. 2019;12:2039–52.